Scientific Calendar December 2023
Suspected nontuberculous mycobacterial (NTM) lung disease
What could be indicators of an underlying infectious cause of pleural effusion?
Elevated WBC counts
Absence of high-fluorescence cell counts
Increased RBC counts
High viscosity of fluid
Congratulations!
That's the correct answer!
Sorry! That´s not completely correct!
Please try again
Sorry! That's not the correct answer!
Please try again
Notice
Please select at least one answer
Scientific background
Nontuberculous mycobacterial infections (NTM)
NTM summarises a group of mycobacteria of ~160 acid-fast staining bacterial species with a ubiquitous appearance. Some of them can cause disease in humans, where the most common manifestation is pulmonary. Clinicians have found an increase in pulmonary infections with NTM over the last two decades which has also increased the public health concern [1].
The involvement of the pleural space for this type of infection is rare [2].
Pleuritis is not a common complication in pulmonary NTM. A retrospective study found proven NTM pleuritis in 1.4% of confirmed pulmonary NTM cases. Pleural effusions were tested for differential cell counts and pathogens. The screening approach for patients with isolated NTM from sputum included patients with pleural effusion and NTM in their study.
A typical finding for the presence of intracellular bacteria is a predominance of lymphocytes in the pleural fluid of NTM pleuritis [3].
In a recent study, only 7 out of 100 NTM patients showed NTM pleuritis [4].
Pleural effusion
Pleural fluid fills the pleural space between the lung and the wall of the chest cavity. It thereby cushions the delicate lung tissue against friction from the ribs and the chest wall. It allows the pleura to glide smoothly during inhalation and exhalation.
A pleural effusion can be very small (and only seen on a chest x-ray or CT scan) or large, containing several litres of fluid. One symptom could be breathing impairment.
Pleural effusions might have a transudative or exudative origin. Transudate means an increased filtration of serum (low-protein), whereas exudates are caused by a leakage or active secretion (high-protein).
Transudate: benign process, the underlying condition might be heart failure or liver failure.
Exudate: evidence of a serious local process like malignancy, infection or trauma.
Cell-based and clinical chemistry parameters support the decision for one of the above reasons. If the exudate criteria are met, the clinical question regarding whether the cause is infectious or malignant should be answered.
Patient case
A male patient in his seventies with a known history of cancer was hospitalised due to continuous chest pain and transient fever. The patient underwent drainage for secondary pneumothorax. The pleural fluid was analysed according to the clinical question of whether or not the cause was ‘infection’. Due to the high proportion of lymphocytes, mycobacteriosis was suspected.
Numerical Results
The pleural effusion sample was analysed in the XR-Series Body Fluid (BF) mode and showed the following results:
Cell count and differential
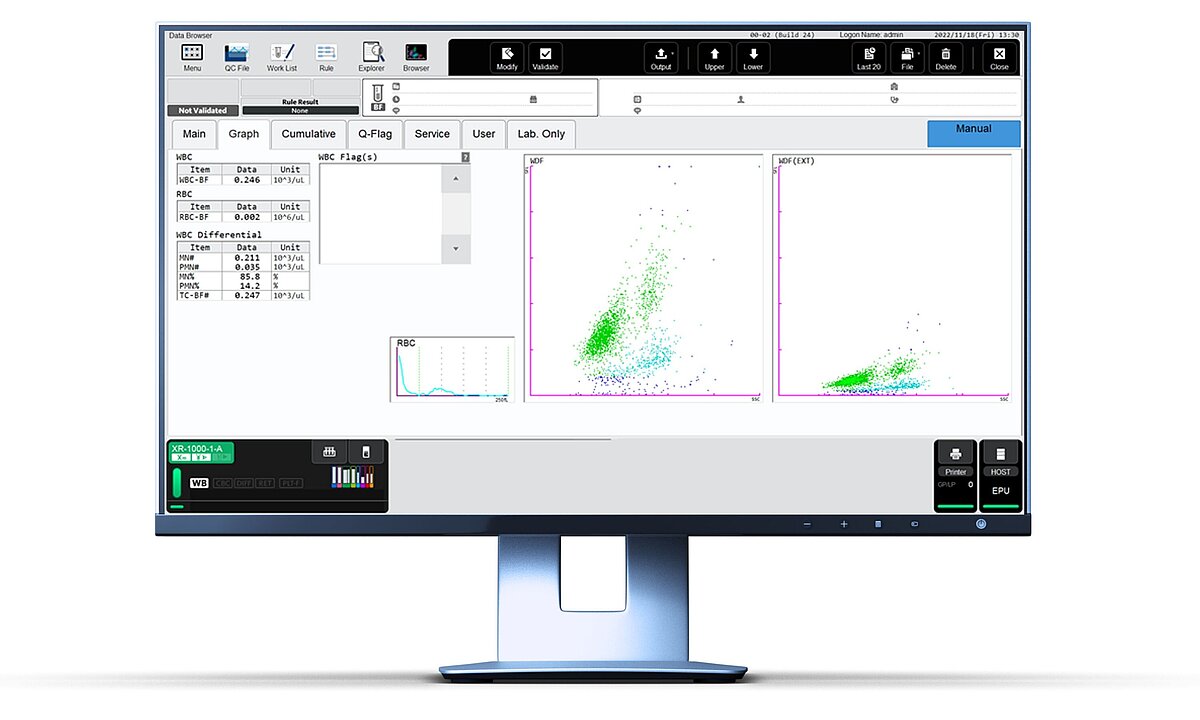
Research parameters
| HF-BF | 1/ µL | ||
| NE-BF# | 35/ µL | NE-BF% | 14.2% |
| LY-BF# | 182/ µL | LY-BF% | 74% |
| MO-BF# | 29/ µL | MO-BF% | 11.8% |
| EO-BF# | 0/ µL | EO-BF% | 0% |
The WDF scattergram in BF mode showed two MN clusters (shown in green): one (lower left) representing lymphocytes and the other (upper right) monocytes. Using cytospin microscopy, numerous lymphocytes (79%) with reactive morphology including dark blue cytoplasm and plasma cell features were identified.
WDF BF 3D scattergram showing two MN clusters (green): representing lymphocytes and monocytes
Additional clinical chemistry and pathogen-specific tests were performed.
Clinical chemistry tests
| Lactate dehydrogenase (LD): | 127 U/L |
| Total protein (TP): | 2.2 g/dL |
| Albumin (ALB): | 1.3 g/dL |
| Glucose (GLU): | 83 mg/dL |
Microbiology and pathogen-specific tests
A tuberculosis-specific ELISPOT test was negative, which is why nontuberculous mycobacterial infection was suspected. In fact, the MAC-PCR test was performed twice, but both results were negative. The cytopathology test was also negative.
Based on the laboratory diagnostic test results, the clinician’s initial suspicion of nontuberculous mycobacterial (NTM) lung disease could not be confirmed.
References
[1] Wassilew N et al. (2016): Pulmonary Disease Caused by Non-Tuberculous Mycobacteria. Respiration. 91(5):386-402.
[2] Ando T et al. (2018): Clinical Features and Prognosis of Nontuberculous Mycobacterial Pleuritis. Respiration. 96(6):507-513.
[3] Park S et al. (2017): Clinical characteristics and treatment outcomes of pleural effusions in patients with nontuberculous mycobacterial disease. Respir Med. 133:36-41.
[4] Wen P et al. (2020): Clinical Relevance and Characteristics of Nontuberculous Mycobacterial Pleuritis. Jpn J Infect Dis. 2020 Jul 22;73(4):282-287.