Scientific Calendar September 2019
Latest generation of haemophilia A treatment – emicizumab
Which assay type is at present the only one to be used for determining the emicizumab concentration?
One-stage APTT-based factor VIII assay
Factor VIII chromogenic assay with coagulation factors of human origin, e.g. BIOPHEN™ Factor VIII:C
Factor VIII chromogenic assay with coagulation factors of bovine origin, e.g. SIEMENS Factor VIII Chromogenic Assa
Congratulations!
That's the correct answer!
Sorry! That´s not completely correct!
Please try again
Sorry! That's not the correct answer!
Please try again
Notice
Please select at least one answer
References
[1] Mannucci PM, Tuddenham EG. The hemophilias – from royal genes to gene therapy. N Engl J Med. 2001; 344(5):1773–1779.
[2] White GC, Rosendaal F, Aledort LM, Lusher JM, Rothschild C, Ingerslev J. Definitions in Hemophilia. Recommendations of the Scientific Subcommittee on FVIII and Factor IX of the SSC of ISTH. Thromb Haemost 2001; 0:560.
[3] Coppola et al. Treatment of hemophilia: a review of current advances and ongoing issues. Journal of Blood Medicine, 2010; 1:183-195.
[4] Hemlibra® – Product Information. Annex 1 – SUMMARY OF PRODUCT CHARACTERISTICS. European Medicines Agency. EMA/162298/2019. First published: 01.03.2018. Last updated: 05.06.2019.
[5] Hemophilia.org, MASAC Recommendation on the Use and Management of Emicizumab-kxwh (Hemlibra®) for Hemophilia A with and without Inhibitors. December 7, 2018.
[6] Oldenburg J, Mahlangu JN, Kim B et al. Emicizumab Prophylaxis in Hemophilia A with Inhibitors. N Engl J Med. 2017; 377:809‐818.
[7] Collins et al. Treatment of bleeding episodes in haemophilia A complicated by a factor VIII inhibitor in patients receiving Emicizumab. Interim guidance from UKHCDO Inhibitor Working Party and Executive Committee. Haemophilia. 2018; 24:344-347.
[8] Paz-Priel et al. Immunogenicity of Emicizumab in People with Hemophilia A (PwHA): Results from the HAVEN 1-4 Studies. Blood 2018; 132:633.
[9] Hemophilia.org, MASAC Safety Information Update on Emicizumab (HEMLIBRA®). April 24, 2018.
[10] Shinohara et al. Evaluation of Emicizumab Calibrator and Controls with a Modified One-stage FVIII Assay on an Automated Coagulation Analyzer. Poster PB1305 presented at the ISTH congress 2019.
[11] Adamkewicz et al. Effects and Interferences of Emicizumab, a Humanised Bispecific Antibody Mimicking Activated Factor VIII Cofactor Function, on Coagulation Assays. Thromb Haemost 2019; 119:1084-1093.
[12] Hemophilia.org, MASAC Update on the Approval and Availability of the New Treatment: Emicizumab (Hemlibra®), for Persons with Hemophilia A with Inhibitors to Factor VIII: Interim Guidance on Acute Bleed Management and Use of Laboratory Assays. November 24, 2017.
[13] Amiral J et al. FVIII and Variant Chromogenic Assays for Measuring Emicizumab and FVIII Inhibitor Antibodies in Human Plasma. Poster PB0228 presented at the ISTH congress 2019.
Scientific background information
Haemophilia A (HA) is a congenital bleeding disorder caused by a deficiency or complete absence of coagulation factor VIII (FVIII). This X-linked disorder represents the majority of the inherited deficiencies of clotting factors, occurring in approximately one per 5,000 male births, without racial predilection. [1] Based on the residual endogenous FVIII concentration HA is classified into three classes (Table 1).
Table 1 Haemophilia classification [2]
Classification | Factor activity | Bleeding tendency |
| Severe | < 1 % of the norm (< 0.01 IU/mL) | Spontaneous bleeding in joints, muscles or gastrointestinal tract |
| Moderate | ≥ 1 to 5 % of the norm (≥ 0.01 to 0.05 IU/mL) | Rare spontaneous bleeding in joints, mostly bleeding after trauma |
| Mild | ≥ 5 to 40% of the norm (≥ 0.05 to 0.40 IU/mL) | Bleeding after injury or surgery, rare bleeding tendency in daily routine |
Although the bleeding phenotype may be rather heterogeneous, even in severe haemophiliacs, this classification reflects the severity of clinical symptoms, with spontaneous joint and muscle bleeds being largely confined to patients with severe haemophilia. [3]
The treatment of HA patients has changed over the decades and brought improvements for those affected. In recent years, (recombinant) FVIII concentrates were the drug of choice; now, with emicizumab, a new generation of HA medication has emerged.
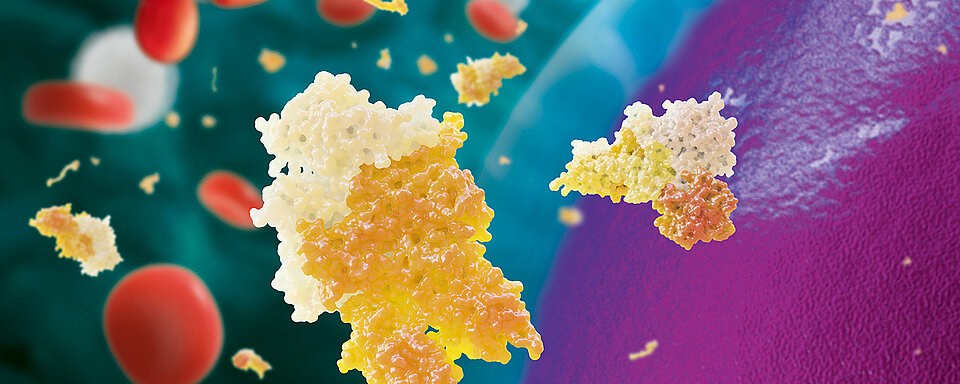
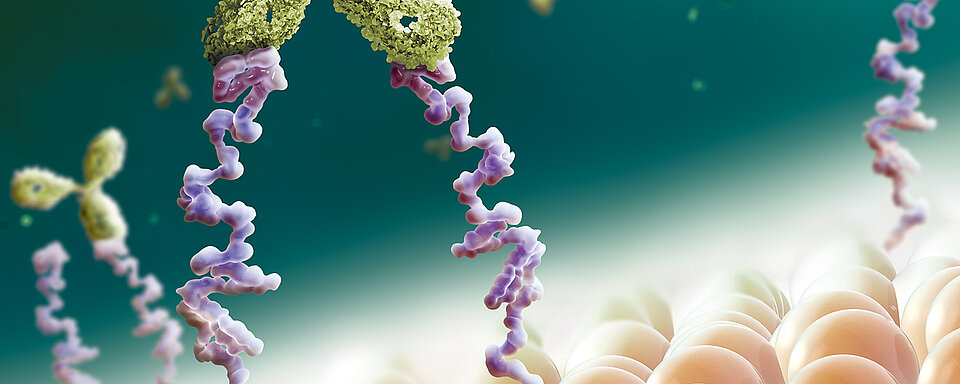
Emicizumab is a humanised, modified, monoclonal immunoglobulin G4 (IgG4) antibody with a bispecific antibody structure. It substitutes for part of the cofactor function of activated factor VIII (FVIIIa) by bridging activated factor IX (FIXa) and factor X (FX) to restore effective haemostasis in HA individuals. It is indicated for routine prophylaxis to prevent or reduce the frequency of bleeding episodes in adults and children of all ages (neonates and older), with and without FVIII inhibitors. The drug has no structural relationship or sequence homology to FVIII, so does not trigger or enhance the development of direct FVIII inhibitors. [4, 5]
Managing emicizumab in clinical practice
After an initial weekly dose of the drug over a period of four weeks, the treatment regimen may be changed to a maintenance dose every two or four weeks. [4] Although emicizumab reduces the frequency of bleeds significantly, bleeding episodes persist under certain conditions, and this may require additional haemostatic treatment with bypassing agents such as activated prothrombin complex concentrate (aPCC, FEIBA®, Shire, Dublin, Ireland), recombinant FVIIa (rFVIIa, Novoseven®, Novo Nordisk, Bagsværd, Denmark), or the substitution of (recombinant) FVIII concentrates. Combined treatment of emicizumab with aPCC has been associated with thrombotic microangiopathy (TMA), venous thrombosis and skin necrosis. [6] To date, no comparable side effects with co-administration of emicizumab and rFVIIa or FVIII concentrates have been observed. But the mechanism that causes TMA and skin necrosis is unclear, and parallel treatment with bypassing agents should be considered carefully or preferably stopped 24 hours before emicizumab is started. [7]
Anti-drug antibody (ADA) formation is commonly observed (e.g. with monoclonal antibodies) and the presence of ADA may alter the pharmacokinetics (PK) and/or pharmacodynamics (PD) and can affect drug efficacy as well as patient safety. During certain clinical studies (e.g. HAVEN 1-4), but also during first routine use, several cases of ADA-positive patients were reported. Even though most of the ADA were transient, few of the ADA were classified as having neutralising potential, which lead to the treatment being discontinued because of the loss of its efficacy. [8]
Regular monitoring of HA individuals under emicizumab treatment is not needed. [4] However, the drug has a long half-life, so the treatment recommendations described in guiding documents should be observed for six months after stopping the drug. [4] This may require additional drug monitoring by lab tests after drug administration has been ended.
Managing emicizumab in laboratory practice
The requirements for a laboratory to test the drug activity are challenging. Activated partial thromboplastin time (APTT) or activated clotting time (ACT) present overly shortened clotting times with emicizumab, which does not require activation by thrombin. One-stage APTT-based FVIII assays show normal or strongly elevated results in HA individuals receiving emicizumab. [4, 9] However, this may be overcome by calibrating the assay with a commercially available emicizumab calibrator in a modified FVIII clotting assay. [10]
A suitable alternative to APTT-based factor assays might be single factor assays utilising chromogenic or immuno-based methods to monitor the coagulation parameters during treatment. FVIII chromogenic assays are manufactured with either human or bovine coagulation proteins. However, both types respond differently to emicizumab.
Since FVIII chromogenic assays with coagulation factors of human origin, e.g. BIOPHEN™ Factor VIII:C (HYPHEN BioMed (a Sysmex Group company), Neuville-sur-Oise, France), are responsive to emicizumab, this assay type is at present the only one to be used for determining the emicizumab concentration. However, results must be considered carefully, as this assay type may overestimate the clinical haemostatic potential of the drug, specifically when measuring endogenous or infused FVIII activity in the presence of emicizumab. [4, 11]
On the other hand, FVIII chromogenic assays with coagulation factors of bovine origin, e.g. SIEMENS Factor VIII Chromogenic Assay (SIEMENS Healthineers, Erlangen, Germany), are unresponsive to emicizumab and may be used to assay endogenous or infused FVIII activity in case of combined therapy with FVIII concentrates. [4, 12] Because emicizumab remains active in the presence of FVIII inhibitors and produces false negative results in clot-based Bethesda tests, bovine-based FVIII chromogenic assays may be used for patients with inhibitors against FVIII, too. [4] Alternatively, a modified BIOPHEN™ FVIII:C assay, in which human FX is replaced with a bovine FX, can be used. [13]
For the time being, there are no commercially available assays for the determination of ADA against emicizumab. Nevertheless, besides the determination of the emicizumab concentration using FVIII chromogenic assays with coagulation factors of human origin, APTT assays and/or one-stage APTT-based assays might provide evidence of the presence of ADA. While evaluating a reported loss of efficacy due to ADA, a prolonged conventional APTT assay and/or a low clot-based FVIII activity in an individual treated with emicizumab is an indicator for the presence of a neutralising ADA directed against emicizumab. [9]
Table 2 summarises the available HA assays and their usability in HA patients under emicizumab treatment. Table 3 summarises the effects of emicizumab on other assays.
Table 2 Usability of haemophilia A assays in individuals treated with emicizumab [4, 10]
Assay | Suggested use in individuals treated with emicizumab |
APTT |
|
One-stage APTT-based FVIII assay |
|
APTT-based Bethesda assays |
|
Activated clotting time (ACT) |
|
FVIII chromogenic assay, bovine origin |
|
FVIII chromogenic assay, human origin |
|
Immuno-based FVIII assays |
|
Table 3 Effect of emicizumab on other assays [10, 11]
Assay | Effect on results |
Fibrinogen (Clauss) | - |
Thrombin Time | - |
One-stage APTT-based factor IX assay | ↑↑ |
Factor IX chromogenic assay | - |
One-stage APTT-based factor XI assay | ↑↑ |
One-stage APTT-based factor XII assay | ↑↑ |
Protein C (clotting) assay | ↓↓ |
Protein C chromogenic assay | - |
Protein S (clotting) assay | ↓ |
Free-Protein S antigen assay | - |
DVRRT assays | - |
Prothrombin Time | - |
One-stage PT-based factor II assay | - |
One-stage PT-based factor V assay | - |
One-stage PT-based factor VII assay | - |
One-stage PT-based factor X assay | - |
FXIII chromogenic assays | - |
Anti-Xa activity assays | - |
Antithrombin assays | - |
Plasminogen activity and antigen assays | - |
D-Dimer assay | - |
vWF activity and antigen assays | - |
↑↑ Severe overestimation
↑ Overestimation
- Not influenced
↓ Underestimation
↓↓ Severe underestimation