Scientific Calendar June 2025
Neutrophils in innate host defence against Staphylococcus aureus infection
How can the parameter NEUT-RI be related to neutrophil activation?
NEUT-RI reflects increased metabolic activity of neutrophils, indicated by increased fluorescence intensity.
NEUT-RI reflects the total neutrophil count.
NEUT-RI represents neutrophils’ cytoplasmic granularity.
NEUT-RI remains unchanged regardless of neutrophil activation.
Congratulations!
That's the correct answer!
Sorry! That´s not completely correct!
Please try again
Sorry! That's not the correct answer!
Please try again
Notice
Please select at least one answer
Scientific Background
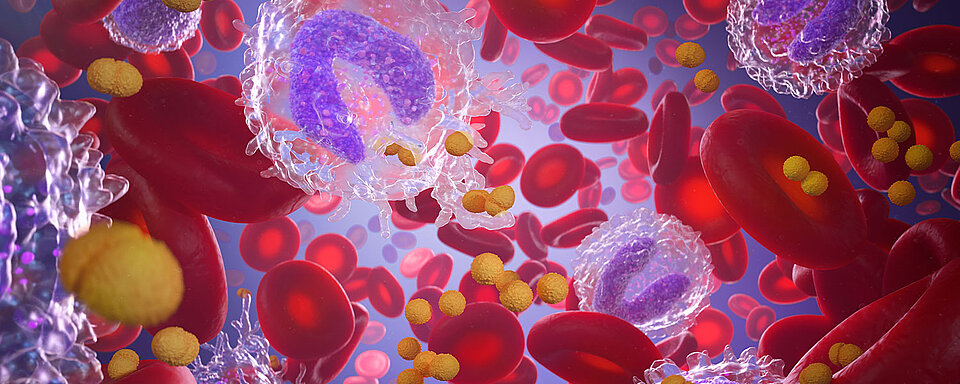
Neutrophils are among the first responders of the innate immune system in combating bacterial infections. Upon the onset of a local infection, systemic inflammation increases the de novo production of neutrophils and enhances the mobilisation of immature neutrophils into circulation [1]. Activated neutrophils migrate from the bloodstream to the infected tissue, where they capture, engulf, phagocytose, and kill invading microorganisms by releasing antimicrobial substances.
Activated and attracted by various cytokines, neutrophils form net-like structures called ‘neutrophil extracellular traps’ (NETs), a process known as ‘NETosis’ [2]. During this process, the neutrophils release nucleic acid, condensed as chromatin, which makes up the main component of NETs, together with histones and numerous proteins [2]. However, besides the benefit of pathogen clearance, excessive NETosis can be detrimental to the host [3]. Moreover, the interaction between NETs, platelets, and the endothelium plays a crucial role in the development of immunothrombosis, contributing to disseminated intravascular coagulation (DIC) and resulting in thrombocytopenia [4, 5].
Obtained from a routine blood count, Sysmex haematology analysers can differentiate between activated neutrophils (neutrophil reactivity intensity = NEUT-RI) and resting neutrophils (NEUT %/#), based on their fluorescence intensity signal. Activated neutrophils produce pro-inflammatory cytokines, and this increased metabolic activity results in higher fluorescence intensity signals [6].
Besides neutrophils, the appearance of immature granulocytes (IG) in the peripheral blood indicates an enhanced demand for neutrophils that exceeds the bone marrow’s maturation capacity, leading to the premature release of progenitor cells into circulation. This provides information about the severity of the innate immune response [7].
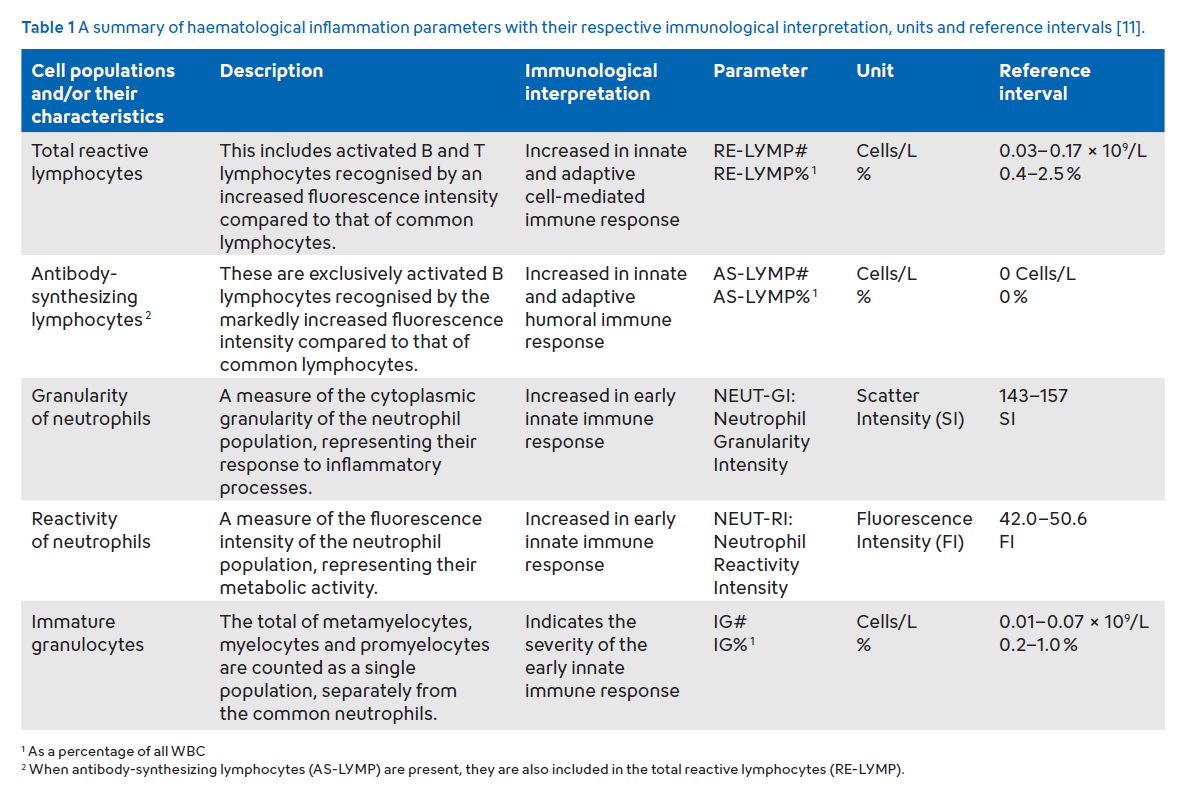
Neutrophil parameters (NEUT-RI, NEUT-GI), along with lymphocyte parameters (RE-LYMP, AS-LYMP), constitute Sysmex’s ‘Extended Inflammation Parameters’ (EIP). This set of diagnostic parameters allows the quantification of the activation status of these cells (Table 1). Different study groups have shown that EIP can support the differentiation of septic and non-septic patients, as well as bacterial and viral infections [8–10].
Case results
A male patient in his 70s was admitted to the hospital for a workup of nephrotic syndrome. During his stay he developed a fever. Blood testing revealed white blood cells (WBC) and red blood cells (RBC) within reference intervals [11]; however, platelets were markedly decreased, and the WBC differential showed neutrophil dominance.
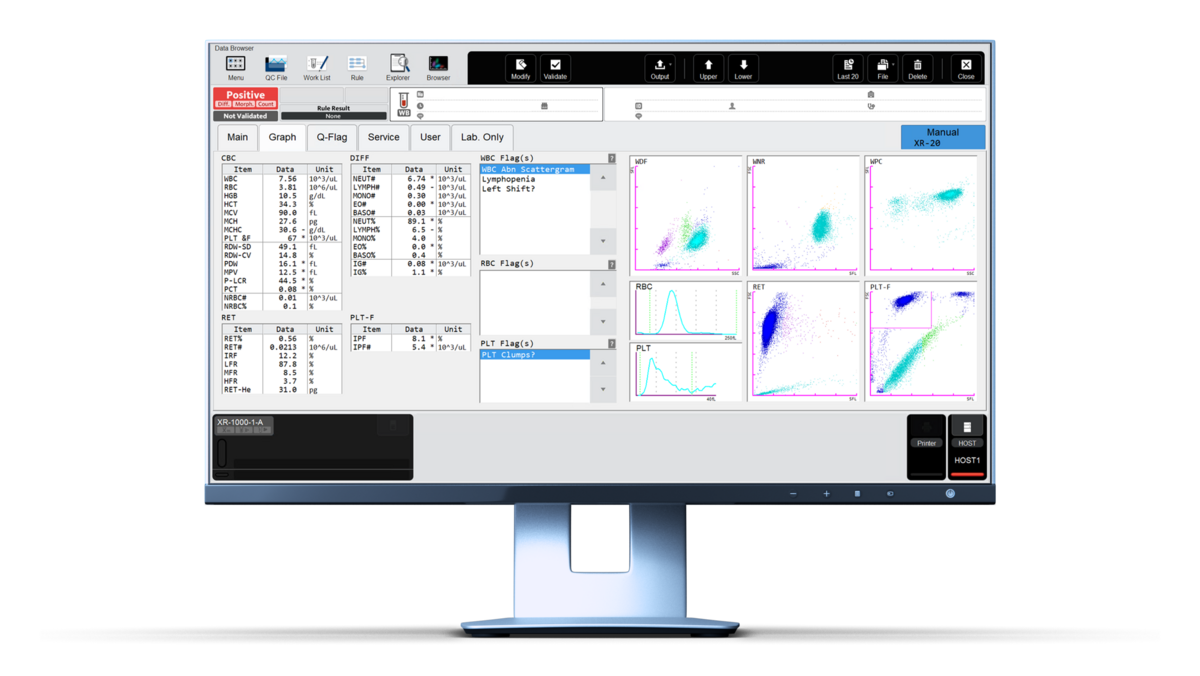
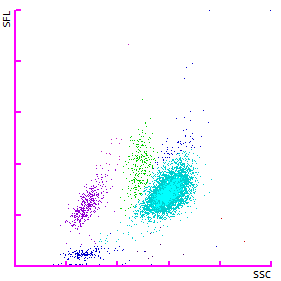
In the WDF scattergram, the neutrophil cloud (light blue) was shifted upwards towards an increased SFL signal (Fig. 2). This observation aligns with the increased NEUT-RI value of 73.3 FI (reference interval: 42.0 – 50.6 FI [11]). Additionally, a subset of cells is classified as immature granulocytes (dark blue) in the WDF scattergram. The elevated neutrophil count, increased neutrophil activation (NEUT-RI), and the increasing immature granulocytes are consistent with the pattern of an early innate immune response against bacterial infections.
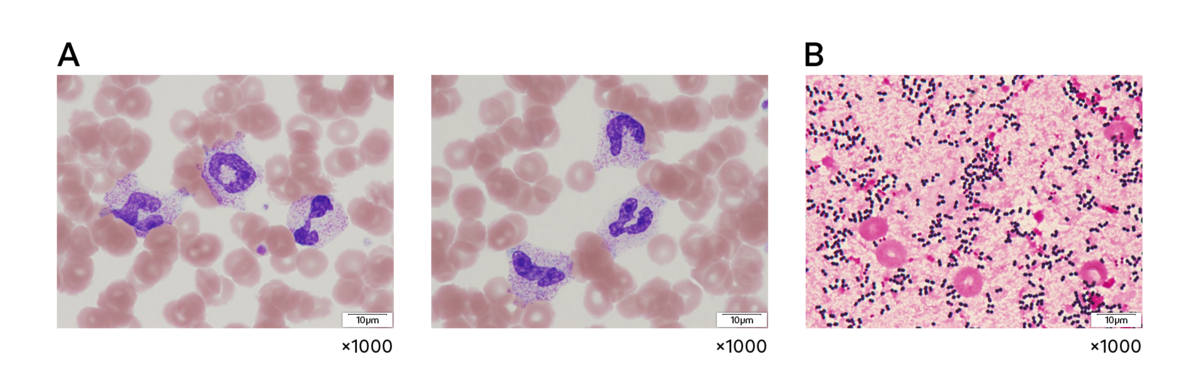
Neutrophil activation was further confirmed by the presence of toxic granulation on the peripheral blood smear. Additionally, the inflammation marker C-reactive protein (CRP) was elevated (40.3 mg/L).
The observed thrombocytopenia (PLT 67 x 103/µL) is a common phenomenon during bacterial inflammation and might be driven by decreased platelet production, increased platelet activation and consumption in thrombi, and heightened platelet destruction [12]. The blood culture was positive and confirmed the occurrence of a bacterial infection with S. aureus.
References
[1] Malech HL et al. (2020): The Role of Neutrophils in the Immune System: An Overview. Methods Mol Biol; 2087:3–10.
[2] Brinkmann V et al. (2004): Neutrophil extracellular traps kill bacteria. Science. 303(5663):1532–1535.
[3] Papayannopoulos V (2021): Neutrophil extracellular traps in immunity and disease. Nat Rev Immunol; 18:134–147.
[4] Zhang H et al. (2021): Tissue factor-enriched neutrophil extracellular traps promote immunothrombosis and disease progression in sepsis-induced lung injury. Front Cell Infect Microbiol; 11:677902.
[5] Chen Z et al. (2021): Review: the emerging role of neutrophil extracellular traps in sepsis and sepsis-associated thrombosis. Front Cell Infect Microbiol; 11:653228.
[6] Mantovani EMA et al. (2023): The Potential Role of Neutrophil-Reactive Intensity (NEUT-RI) in the Diagnosis of Sepsis in Critically Ill Patients: A Retrospective Cohort Study. Diagnostics (Basel); 13(10):1781.
[7] Nierhaus A et al. (2013): Revisiting the white blood cell count: immature granulocytes count as a diagnostic marker to discriminate between SIRS and sepsis–a prospective, observational study. BMC Immunol; 14:8.
[8] Herawati S et al. (2024): Integrating Routine Hematological and Extended Inflammatory Parameters as a Novel Approach for Timely Diagnosis and Prognosis in Sepsis Management. Diagnostics (Basel); 14(9):956.
[9] Park SH et al. (2015): Sepsis affects most routine and cell population data (CPD) obtained using the Sysmex XN-2000 blood cell analyzer: neutrophil-related CPD NE-SFL and NE-WY provide useful information for detecting sepsis. Int J Lab Hematol; 37(2):190–198.
[10] Urrechaga E et al. (2018): Neutrophil Cell Population Data biomarkers for Acute Bacterial Infection. Journal of pathology and infectious Diseases; 1(1):1–7.
[11] L van Pelt J et al. (2022): Reference intervals for Sysmex XN hematological parameters as assessed in the Dutch Lifelines cohort. Clin Chem Lab Med 60(6):907–920.
[12] Wilson JJ et al. (1982): Infection-induced thrombocytopenia. Semin Thromb Hemost; 8(3):217–233.